Safety of our patient and quality of care are of utmost importance. For this reason we require specimens sent to the Spectrum Health Cytology Laboratory be labeled with at least two patient identifiers, (i.e., patient legal name, birth date and MRN.) We will no longer return to the collection site, unlabeled, mislabeled specimens lacking two patient identifiers or specimen containers with multiple different patient labels. These specimens will be discarded and repeat collection will be necessary.
Procedures to verify correct labeling of patient specimens at the time of collection are recommended. Specimen containers should not be pre-labeled. Variation of the “time-out” procedure used in the hospital and surgical center setting is an excellent way of confirming that the specimen is correctly labeled. This can easily be achieved by having the patient verify his or her name and birth date, by reading the label placed on the specimen container at the time the specimen is collected. This “time out” should occur before the specimen leaves the examination or treatment room.
It is our mission to provide the best and safest care we can to our patients. We know that physicians and other practitioners are required to see patients more efficiently and at times with less than adequate time allowed. Following a “time out” procedure and not pre-labeling specimen containers will prevent errors that may lead to diagnoses being assigned to wrong patients, hence, unnecessary procedures and lack of follow-up for the appropriate patient.

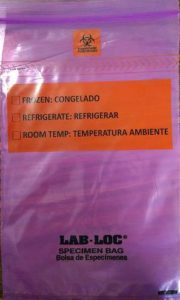 Spectrum Health Regional Laboratory supplies purple priority bags for specimens that must be handled and processed immediately upon receipt in the laboratory. The purple color priority transport bag will be a visual cue to the receiving laboratory that the specimens inside the bag need to be handled or processed immediately at the time of arrival in the laboratory or the integrity of the specimen will be compromised.
Spectrum Health Regional Laboratory supplies purple priority bags for specimens that must be handled and processed immediately upon receipt in the laboratory. The purple color priority transport bag will be a visual cue to the receiving laboratory that the specimens inside the bag need to be handled or processed immediately at the time of arrival in the laboratory or the integrity of the specimen will be compromised.